
Revolutionizing Healthcare in Kenya & Nepal: Standardizing Data Exchange for Optimal Delivery
- LocationKenya and Nepal
- ImplementationFebruary 2024 - Present
Leveraging Interoperability to Enhance Patient Care Across Africa and Asia
As patients move across different points of care within the healthcare system, their data is stored either on physical files or digitally. Recently, governments around the world began advocating for the use of digital systems for patient care delivery and data storage. However, if these systems do not effectively exchange data, patients’ health records can become inaccessible, hindering care as patients move between home and the health facility. The lack of interoperability and standardization in most health systems means data from one system cannot be automatically consumed by others within the digital health ecosystem. This may force systems to interact through tightly coupled peer-to-peer data exchange mechanisms, making data exchange at scale difficult to manage.
Establishing a scalable strategy is most achievable when utilizing an interoperable, standards-based data exchange as opposed to directly linking individual systems to share data. A strategy for interoperability can scale to support practices that improve care coordination, reduce medical errors, and increase the efficiency of care delivery.
As the technical steward and core contributor to the Community Health Toolkit (CHT), Medic advances equitable care in solidarity with technical organizations, governments, and NGOs, serving hard-to-reach communities.
Community health workers (CHWs) are the primary users of the Community Health Toolkit (CHT) as they administer care to patients at household level. The data collected on the application is subsequently synced to central servers for analysis. There are a number of users at this level, including policy makers and data analysts, who use other systems to process this data. The result is a critical need to standardize the data coming from the CHT and other systems.
- Ministry of Health Kenya
- SunyaEK
- Medic

Facility-based systems or data aggregation systems within the ecosystem exchange data with the CHT according to what workflows are used at the different points of care. These systems collect data that needs to be aggregated or exchanged for visualization on standard dashboards. This fragmentation poses obstacles for healthcare providers seeking to access and exchange patient information for continuity of care. Adopting a standard for exchanging data with other systems offers the opportunity for easier integration to support data use across systems and better support continuity of care.
By enabling different health systems and applications to communicate with each other, interoperability increases the efficiency of healthcare delivery.
Impact
-
Exchanging Data at a National Sclae
2023:
Kenya’s Ministry of Health adopted the CHT for national scale across the various counties as it can exchange data with various systems across the digital health ecosystem
The CHT bidirectionally exchanges data with the national shared health record within the digital health ecosystem.
-
Client Registry and CHT Harmony
2024:
In collaboration with various partners, the Kenyan Ministry is developing a client registry that will exchange data with the CHT as the single source of truth. This will be based on FHIR standards.
-
163,000 Community Health Workers Supported
The Community Health Toolkit (CHT) to date is:
Supporting 163,000 community health workers
Active across 18 countries
Reaching an estimated 80 million people
-
Reduced Cost of Care and Improved Efficiency
In Nepal, Medic and SunyaEK partnered to deploy the CHT and OpenMRS that will exchange FHIR standardized patient data leveraging the reference application built by Medic. Utilizing the reference application saved on time, leading to prompt delivery, reduced cost of care and improved efficiency of the caregivers.

- The data structure of the CHT required a significant amount of effort in the beginning in order to comply with FHIR standards, with the majority of the work going into mapping the indicators and building the first mediators that could be reused or expanded to suit other emerging requirements.
- The use of open standards holds many advantages, as it is highly scalable. Medic was able to leverage the work done on the initial proof of concept for all the subsequent projects in Kenya and Nepal.
The Approach
To ensure interoperability amongst the disparate systems within the digital health ecosystem, the team harnessed the capabilities of OpenHIE architecture, including the interoperability services layer, and used various FHIR resources such as Patient, Encounter, Subscription, Organization and Endpoint.
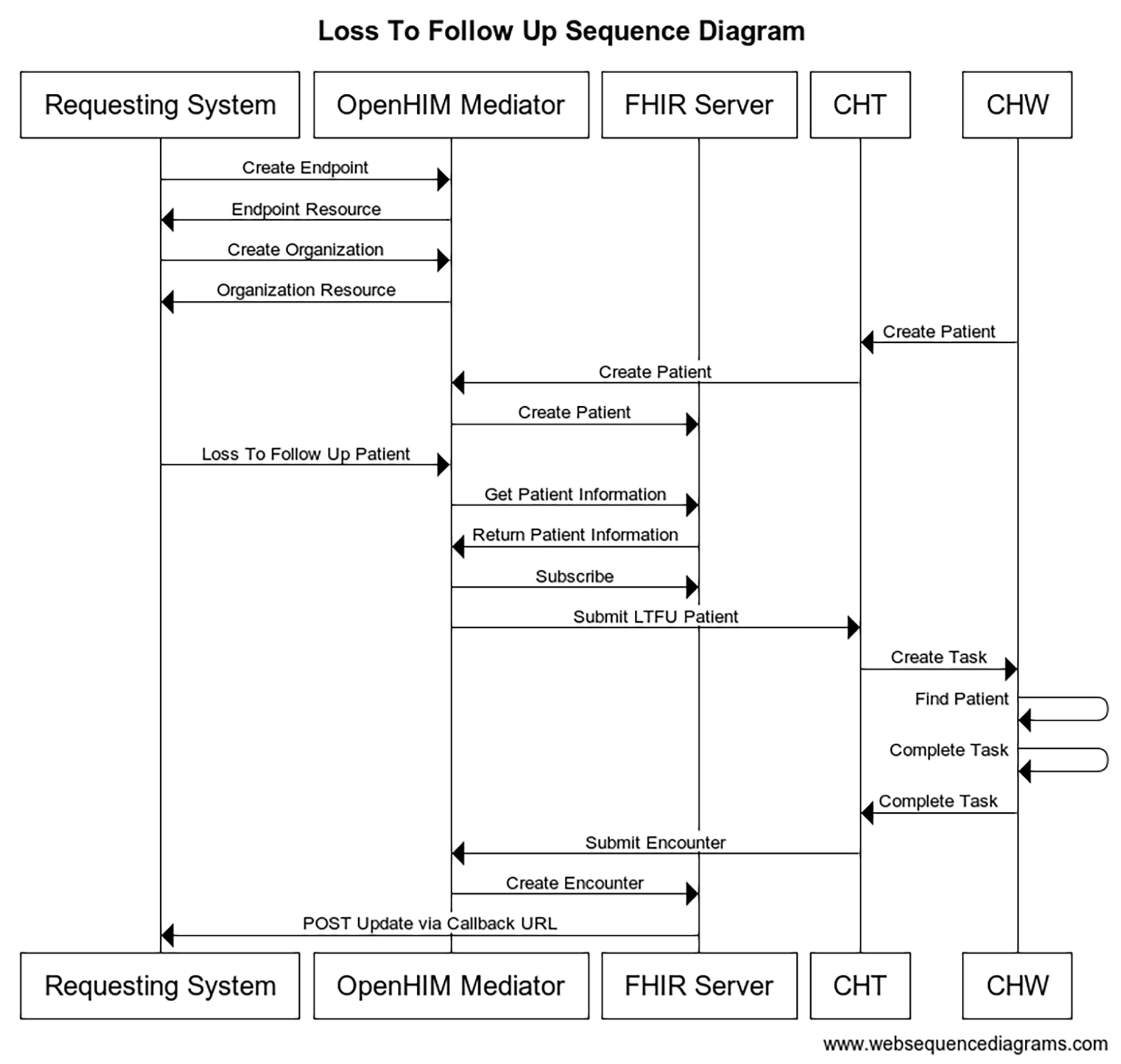
Figure 2: Shows the actions on the different systems to complete a loss to follow up workflow.
In 2024, Medic reached the milestone of 130,000 community health workers supported globally by the CHT to deliver care. The CHT empowers the CHWs to provide critical health services including antenatal care, postnatal care, immunizations and many more. With such a substantial user base, vast amounts of data were generated and stored on mobile devices and synchronization servers, providing the need to have a scalable and sustainable way of data exchange (interoperability) between the CHT and other systems.
Having recognized the fragmented nature of care delivery across different points such as health facilities, households, and workplaces, leading to data isolation in disparate systems, Medic ensured that the CHT could send out data that can be interpreted by other systems, and in turn could understand the data it receives.
Medic identified the Loss to Follow Up (LTFU) workflow as a proof of concept use case. The workflow follows a patient who has missed an appointment and a CHW is requested to follow up at household level. The proof of concept workflow is showcased in this “Loss to Follow Up Sequence Diagram” (Figure 2).
-
OHIE Capabilities
- Health worker and patient alerting
- Disease surveillance and reporting
- Tracking and management health worker capabilities and geographic coverage
-
HEALTH ISSUES ADDRESSED
- Individual Patient Care (clinical) – Reproductive, maternal, newborn, and child health
- Individual Patient Care (Clinical) – HIV disease management
- Healthcare Administration – Health Workers
- Healthcare Administration – Health medicine supplies
- Healthcare Administration – Health coverage and enrollment
-
OHIE Workflows
- Send health worker alert workflow
- Query health worker and/or facility records workflow